Okay, let’s be real. The first time I stared at a nutrition label after my diabetes diagnosis, I felt like I needed a PhD in… well, something. Tiny numbers, percentages that made my head spin, and words like “monounsaturated” – what even is that? It was like trying to decipher an alien language.
I remember one time, early on, I grabbed what I thought was a healthy snack bar. It said “low sugar” on the front in big, friendly letters. Perfect, right? I practically inhaled it. Two hours later, my blood sugar was doing the tango, and I was feeling… less than stellar. Turns out, that “low sugar” bar was PACKED with other carbs that my body just couldn’t handle. Lesson learned: the front of the package is basically advertising. The real story is hiding on the back.
So, how do we make sense of this nutritional hieroglyphics, especially when our blood sugar’s happiness depends on it? Don’t worry, I’ve been there, done that, and spilled a few low-carb protein shakes along the way. This is your friendly, slightly-clumsy guide to navigating those labels like a pro (or at least, like someone who mostly knows what they’re doing).
Step 1: The Serving Size Sneak Attack

This is where the food companies get sneaky. At the very top of the label, you’ll see “Serving Size” and “Servings Per Container.” This is crucial. All the other numbers on the label – calories, carbs, everything – refer to that one serving size.
And here’s the kicker: sometimes, the serving size is ridiculously small. Like, “1/2 cup” of cereal? Who eats half a cup of cereal? My cat eats more than that! (Okay, maybe not, but you get the idea.)
So, the first thing you must do is compare the serving size on the label to the amount you’re actually going to eat. If you’re having a whole cup of that cereal, you need to double all those numbers on the label. Yes, all of them. My advice? Get yourself some measuring cups and actually measure out a serving a few times. It’s eye-opening (and sometimes a little depressing, I’ll admit).
Step 2: Calorie Clues (But Not the Whole Story)

Next up: Calories. This tells you how much energy you’re getting from that serving. While the quality of calories (where they come from) is ultimately more important for diabetes management, the total calorie count is still useful, especially for managing your weight – which is often a big part of the diabetes puzzle.
Forget that generic 2,000-calorie-a-day advice. Your needs are personal. Here’s a simplified way to get a ballpark figure for your daily calorie needs, but remember, it’s just a starting point.
First, we need to figure out your Basal Metabolic Rate (BMR). Think of this as the energy your body burns just by existing – breathing, keeping your heart beating, all that essential stuff. A very rough estimate is to multiply your weight in pounds by 10 if you’re a woman, or by 11 if you’re a man.
Then, we factor in your activity level. Be honest with yourself here! If you’re mostly sedentary (little to no exercise), multiply your BMR by 1.2. If you’re lightly active (maybe you walk a few times a week), multiply by 1.375. For moderately active folks (exercising 3-5 days a week), use 1.55. If you’re very active (working out most days), use 1.725. And if you’re extra active (think intense workouts and a physically demanding job), go with 1.9.
Let’s do an example: Imagine a 150-pound woman who’s lightly active. Her BMR would be roughly 1500 calories (150 pounds x 10). Then, because she’s lightly active, we multiply that by 1.375, giving us an estimated daily calorie need of around 2063 calories.
Important Caveat: This is a rough estimate. Things like your age, how much muscle you have, and any underlying health conditions can all affect your actual calorie needs. If you want a precise number, it’s best to talk to a registered dietitian or your doctor. They can give you personalized advice. The main takeaway here is to be mindful of the calorie count on the label and how it roughly compares to your estimated daily needs.
Step 3: The Carb Conundrum (This is Where It Gets Real)
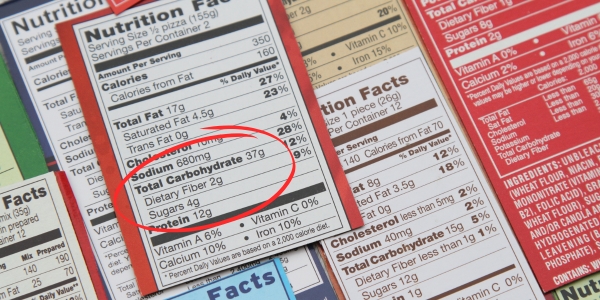
Okay, deep breaths. This is the section that really matters for us folks with diabetes. Carbohydrates are what make our blood sugar go up, so we need to be carb detectives.
You’ll see “Total Carbohydrate” on the label. That’s the big number, the one we really care about. But then, it gets broken down further…
-
Dietary Fiber: Aim high! Fiber helps slow down sugar absorption, preventing those dreaded spikes. A general guideline is 25-38 grams per day, but prioritize foods where fiber makes up a significant portion of the total carbs. Think of it this way: if a food has 20g of total carbs and 5g of fiber, that’s a better ratio than a food with 40g of total carbs and only 2g of fiber.
-
Total Sugars: This includes natural sugars (like in fruit) and added sugars. While natural sugars in whole foods come with other nutrients, it’s still wise to be mindful of the total amount.
-
Added Sugars: Minimize these! Added sugars are the main culprits for rapid blood sugar increases. There’s no magic number, but less is always better. Aim to keep added sugars to a small fraction of your total daily carbohydrate intake. The American Heart Association suggests no more than 25g (6 teaspoons) of added sugar per day for women and 36g (9 teaspoons) for men. For diabetes management, even lower is often beneficial.
-
Sugar Alcohols: These sugar substitutes (sorbitol, xylitol, erythritol, maltitol) have varying effects. Erythritol generally has the least impact, while maltitol can raise blood sugar more significantly. Remember, “sugar-free” doesn’t mean “carb-free,” and these can still affect you.
My personal rule of thumb? I always look at the total carbohydrate number first. That’s the one I use for figuring out my insulin dosage (if you’re on insulin, of course). Then, I glance at the added sugars and try to keep that number as low as humanly possible.
Step 4: Fat Facts (The Good, the Bad, and the Ugly)
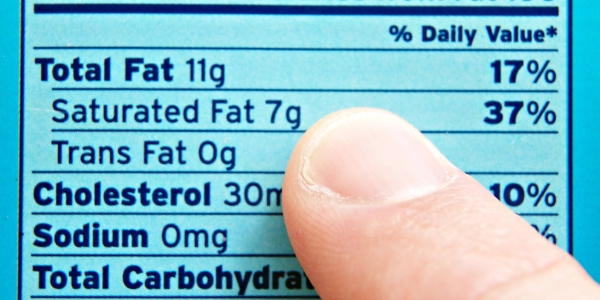
Fats get a bad rap, but they’re not all evil. We actually need some fat in our diet. The key is to choose the right kinds of fat.
Saturated Fat: The One to Limit Strictly
This type of fat is linked to an increased risk of heart disease, which is already a bigger concern when you have diabetes. The American Heart Association recommends keeping saturated fat below 6% of your total daily calories. What does that look like in grams?
- 1,500-calorie diet: Less than 10 grams of saturated fat.
- 2,000-calorie diet: Less than 13 grams of saturated fat.
- 2,500-calorie diet: Less than 17 grams of saturated fat.
Always check the %DV on the label and aim for low percentages. This is your maximum – aim to stay well below it.
Trans Fat: The One to Avoid Completely
This is the worst type of fat. No debate. It’s terrible for your heart and overall health. Thankfully, it’s mostly gone from processed foods, but always check the label. Your target is simple: 0 grams. No exceptions.
Monounsaturated and Polyunsaturated Fats: The Good Guys
These are the fats you want in your diet. They can actually improve your heart health. There’s no strict upper limit, but the goal is to make these the majority of your fat intake.
- Good sources of monounsaturated fats: Olive oil, avocados, nuts (like almonds, cashews, and pecans), and nut butters.
- Good sources of polyunsaturated fats: Fatty fish (salmon, tuna, mackerel), flaxseeds, chia seeds, walnuts, and sunflower seeds.
The label will usually list the total fat and then break it down into these categories. Again, focus on keeping the saturated and trans fats low.
Step 5: Sodium: The Sneaky Salt Shaker
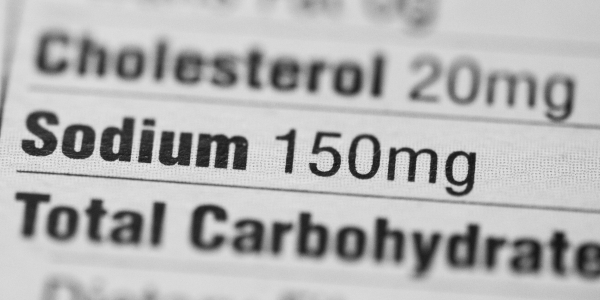
Sodium (salt) is another one to watch, especially if you have high blood pressure (which, again, is common with diabetes). Too much sodium can raise your blood pressure, which is bad news for your heart and kidneys.
The general recommendation is to keep sodium under 2,300 milligrams per day. But honestly, a lot of processed foods are loaded with sodium, so it’s easy to go over that limit without even realizing it. Check the labels, and try to choose lower-sodium options when you can. There are a lot of hidden names for it, too, so do a little research!
Step 6: The Percentage Puzzle (%DV)
Okay, I’m going to be honest: I used to completely ignore those little percentages on the right side of the label (% Daily Value). They seemed confusing and… well, unnecessary.
But, they can actually be pretty helpful. The %DV tells you how much of a particular nutrient that serving of food provides, based on a 2,000-calorie diet.
Here’s a simple rule:
- 5% DV or less = Low
- 20% DV or more = High
So, for things like saturated fat, sodium, and added sugars, you want to aim for a low %DV. For things like fiber, vitamins, and minerals, you want a high %DV.
Step 7: Label Lingo Decoded (and Common Myths Busted!)

Food companies love to slap all sorts of claims on their packages: “Low Fat!” “Sugar-Free!” “Heart Healthy!” But what do those claims actually mean?
| Label Claim | Definition (per standard serving size) |
| Fat-free | Less than 0.5 gram (g) of fat |
| Low fat | 3 g of fat or less |
| Reduced fat | At least 25% less fat than the regular product |
| Saturated fat free | Less than 0.5 grams of saturated fat |
| Low saturated fat | 1 gram (g) or less of saturated fat |
| Trans fat free | Less than 0.5 grams of trans fat |
| Cholesterol free | Less than 2 milligrams (mg) cholesterol and 2 g or less of saturated fat |
| Low cholesterol | 20 mg or less of cholesterol |
| Reduced cholesterol | At least 25% less cholesterol and 2 g or less of saturated fat |
| Sodium-free or salt-free | Less than 5 mg per serving |
| Very low sodium | 35 mg or less of sodium per serving |
| Low sodium | 140 mg or less of sodium per serving |
| Reduced1 or less sodium | At least 25% less sodium than2 the regular version |
| Sugar-free | Less than 0.5 grams (g) of sugar |
| Reduced sugar | At least 25% less sugar than the regular product |
| No sugar added or without added sugars | No sugar or sugar-containing ingredient is added during processing |
| Calorie free | Less than 5 calories |
| Low calorie | 40 calories or less |
| Light or lite | 1/3 fewer calories or 50% less fat than the regular food |
| High fiber | 5 grams (g) or more of fiber |
| Good source of fiber | 2.5 to 4.9 grams (g) of fiber |
It’s good to know what these terms mean, but don’t rely on them alone. Always, always flip the package over and read the full nutrition label. A candy bar might be “fat-free,” but it could still be loaded with sugar!
Common Misconception: “Sugar-free” automatically means “carb-free” or “healthy for diabetes.” This is FALSE! Always check the total carbohydrate content, as sugar-free products can still contain other carbohydrates that affect blood sugar.
Step 8: The Ingredient Inquisition
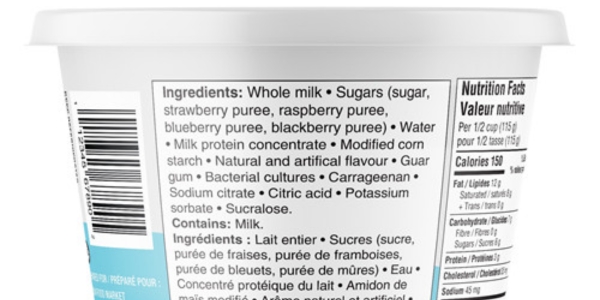
The ingredient list is usually below the rest, and it’s in order from the most used ingredient to the least. This can be really insightful because you can tell if there are a bunch of additives you can’t pronounce, or if the sugar is super high up on the list.
Step 9: Beyond the Label: GI and GL (Optional Extra Credit)

Okay, this is getting into slightly more advanced territory, but it’s worth mentioning. The Glycemic Index (GI) and Glycemic Load (GL) are ways of measuring how quickly a food raises your blood sugar.
- Glycemic Index (GI): This ranks foods on a scale of 0 to 100, based on how they compare to pure glucose. Low-GI foods (55 or less) are digested more slowly and cause a more gradual rise in blood sugar. High-GI foods (70 or higher) cause a faster spike.
- Glycemic Load (GL): This takes into account both the GI and the amount of carbs in a serving. It’s arguably a more accurate measure of a food’s impact on your blood sugar.
You won’t find GI or GL on nutrition labels. You have to look them up online or in a book. And honestly, it can get a little complicated. Some people find it helpful, but others find it too much to keep track of. The American Diabetes Association even says that it is not definitive whether it will reduce diabetes risk. It’s up to you whether you want to delve into this.
Glycemic Index (GI) and Glycemic Load (GL) Categories
| Category | Glycemic Index (GI) | Glycemic Load (GL) |
| Low | 55 or less | 10 or less |
| Medium | 56 to 69 | 11 to 19 |
| High | 70 or higher | 20 or more |
Putting it All Together: Meal Planning with Label-Reading Superpowers

So, you’ve become a label-reading ninja. Now what? Let’s talk about how to use this knowledge to plan meals that keep your blood sugar happy.
- Balance is Key: Aim for meals that combine carbohydrates with protein and healthy fats. This helps slow down the absorption of carbohydrates and prevent those spikes. For example, instead of just eating a bowl of pasta (high carb), add some grilled chicken (protein) and a side salad with olive oil and vinegar dressing (healthy fats).
- Focus on Whole Foods: Whenever possible, choose whole, unprocessed foods over packaged and processed ones. Think fruits, vegetables, lean proteins, and whole grains. These foods tend to be naturally lower in added sugars, sodium, and unhealthy fats.
- Plan Ahead: When you have time, plan out your meals for the week. This makes it easier to make healthy choices and avoid impulse decisions when you’re hungry and short on time.
- Pre-Portion Snacks: If you’re prone to overeating (like I am!), pre-portion your snacks into small bags or containers. This helps you control your portions and avoid mindlessly munching.
- Don’t Be Afraid to Experiment: Finding what works best for your body takes time and experimentation. Pay attention to how different foods affect your blood sugar, and adjust your meal plan accordingly.
The Bottom Line (and a Little Pep Talk)
Look, I know this is a lot of information. It takes time to get the hang of reading nutrition labels, and it’s okay to feel overwhelmed at first. Don’t try to become an expert overnight. Start small. Pick one or two things to focus on – maybe it’s just checking the serving size and the total carbs, or maybe it’s looking for added sugars.
And remember, it’s not about perfection. It’s about making informed choices, most of the time. We all slip up sometimes. We all have days when we eat that “low sugar” snack bar and regret it later. It’s okay. Just dust yourself off, learn from it, and keep going.
You’ve got this! And if all else fails… well, there’s always that dietitian appointment you can make. 😉 (And maybe hide the evidence of the snack bar incident.)
References
- Effects of Lifestyle Intervention in Subjects With Impaired Glucose Tolerance, on Changes in Dietary Intake and Physical Activity, and Associations of These Changes With Metabolic Syndrome Status:
- Efficacy and safety of low-carbohydrate diets: a systematic review and meta-analysis of randomized controlled trials
- Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base
- Food Label Use and Awareness of Nutritional Information and Recommendations among Adults in the United States: A Comprehensive National Survey
- Impact of low-fat diet on cardiometabolic risk factors in patients with type 2 diabetes mellitus: A systematic review and meta-analysis
- Association Between Dietary Sodium Intake and Cardiovascular Outcomes in a Prospective Cohort of Patients With Type 2 Diabetes.
- Food Label Use and Its Relation to Dietary Intake among US Adults: Results from the National Health and Nutrition Examination Survey
- Usefulness of Glycemic Index and Glycemic Load in the Clinical Management of Diabetes
- Systematic review of the effect of personalized nutrition on health